What is rheumatoid arthritis? (RA)-
RA is a characterized by progressive damage of synovial-lined joints and also chronic inflammation. It is thus a progressive disease.Moreover, It is associated with variable extra-articular manifestations. In early disease, Tendon and bursal involvement are also frequently seen. It usually occurs in 4th-5th decade. It is more common in women.
Which area gets affected?
RA can affect any joint, however, metacarpophalangeal, proximal interphalangeal and metatarsophalangeal joint are the most commonly affected. Moreover, the wrists and knee might also get involved. The rarely involved joints include distal interphalangeal, the sacroiliac, and the lumbar spine joints.
Pathological insights-
It is a chronic autoimmune disease. It leads to progressive articular damage, functional loss, and thus significant comorbidity. Presence of Cytokine inhibitors and also interleukin 6 play an evident role in disease pathogenesis. Moreover, Genetic triggers along with environmental factors contribute to the etiopathology.
Clinical features seen-
Intra articular
Extra articular
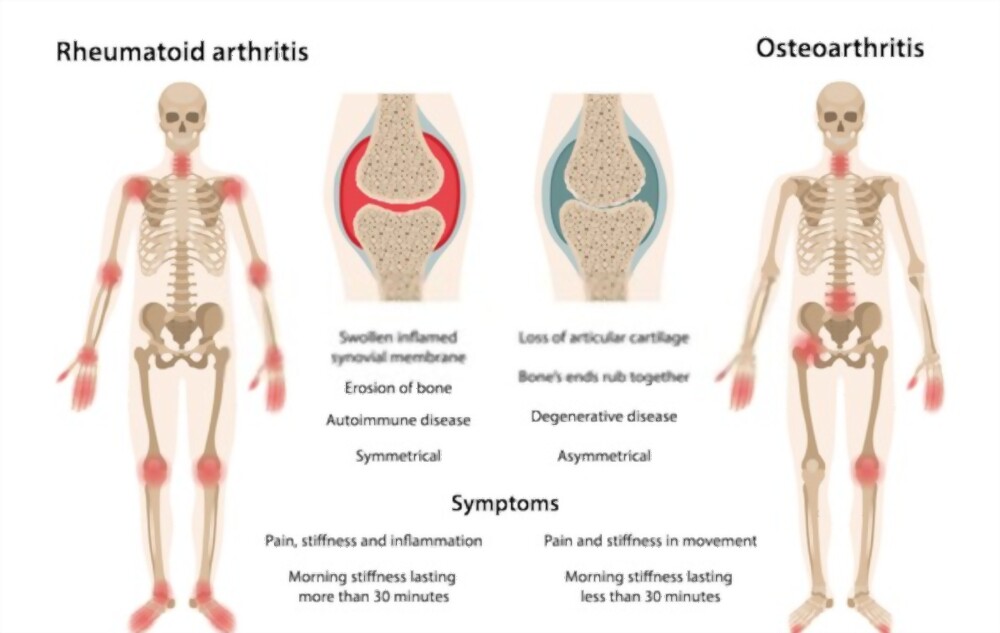
Clinical manifestations include joint swelling and tenderness to palpation. Morning stiffness is the characteristic feature of RA. Morning stiffness usually arises in and around the joints and lasts for an hour. It is important to understand the difference between pain and stiffness. Also, The joints affected show severe restriction in range of motion.
The clinical presentation varies, however the most frequent finding is an insidious onset of pain with symmetric swelling of small joints, however RA also includes palindromic onset and monoarticular presentation.
The general symptoms of RA include malaise, fatigue, weight loss, fever, etc.. Morning stiffness duration depends on the disease activity.
Extra-articular involvement such as nodules, vasculitis, hematologic abnormalities, felty’s syndrome and visceral involvement may also be seen in a few cases.
Risk Factors for developing RA-
Include:
- Increased prevalence of RA within families
- Increases risk: Female sex;
- exposure to occupational dust (silica);
- air pollution;
- low vitamin D
- smoking
- obesity
- Deceased risk:
- fish and omega 3 fatty acid use
- healthy diet
Diagnosis-
Laboratory
Radiology
USG
- Laboratory
Although there is no laboratory test to exclude diagnosis of rheumatoid arthritis, laboratory abnormalities for systemic inflammation can be detected. These include-
- ESR
- Acute phase proteins
- Plasma viscosity
- C-reactive protein(CRP)
- Xray findings- Plain film radiography may show soft tissue swelling and also mild juxtaarticular osteoporosis
- USG – detects tendon and bursal involvement in RA.
How is RA different from OA?
Nutritional guidelines for RA-
Dietary interventions help in reducing disease symptoms.
- Avoiding food that causes inflammation. Examples- processed food, high salt, oils, sugar.
- Supplements: ensure proper intake of vit D cod liver oil, and multivitamins.
Conclusion-
The natural history of the disease is poorly defined. Also the clinical course is fluctuating. Also the prognosis remains unpredictable. RA leads to a relevant cause of disability. An adequate early treatment of RA may help alter the disease course.