The heart’s ability to maintain a steady rhythm is crucial for circulation and overall health. However, conditions like bradycardia, tachycardia, and heart block can disrupt this rhythm, leading to dizziness, fatigue, and even life-threatening complications. When medications and lifestyle changes are insufficient, pacemakers provide an effective solution to restore normal heart function.
Recent innovations in pacemaker technology, including leadless designs, conduction system pacing, and wireless cardiac devices, are enhancing the safety, efficiency, and personalization of heart rhythm management. This article explores the heart’s natural rhythm, when pacemakers become necessary, and the latest technological advancements improving patient outcomes.
The Heart’s Electrical System and Rhythm Disorders
The heart beats due to electrical signals generated by the sinoatrial (SA) node, the body’s natural pacemaker. These signals travel through specialized conduction pathways, ensuring synchronized contractions of the atria and ventricles. Any disruption in this process can result in an arrhythmia, which can be classified into three primary types:
• Bradycardia – A slow heart rate that may cause fainting, fatigue, and shortness of breath.
• Tachycardia – A fast or irregular heartbeat, increasing the risk of stroke or heart failure.
• Heart Block – A delay or blockage in the electrical signals, leading to uncoordinated heartbeats.
In cases where arrhythmias severely affect blood circulation and daily life, medical intervention—such as pacemakers—becomes necessary.
When is a Pacemaker Required?
Doctors recommend pacemakers when the heart’s electrical system fails to function properly, often due to conditions such as:
• Symptomatic Bradycardia – A dangerously slow heart rate that causes persistent dizziness or fainting.
• Heart Block – Particularly third-degree (complete) heart block, where electrical impulses do not reach the ventricles.
• Atrial Fibrillation with Slow Ventricular Response – An irregular heart rhythm that leads to inadequate blood circulation.
• Post-Surgical Recovery – Some patients need temporary pacemakers after heart surgeries or procedures.
The decision to implant a pacemaker is based on a comprehensive evaluation, including electrocardiograms (ECGs), Holter monitoring, and stress tests to assess the severity of the heart rhythm disorder.
Types of Pacemakers and Recent Innovations
Traditional Pacemakers
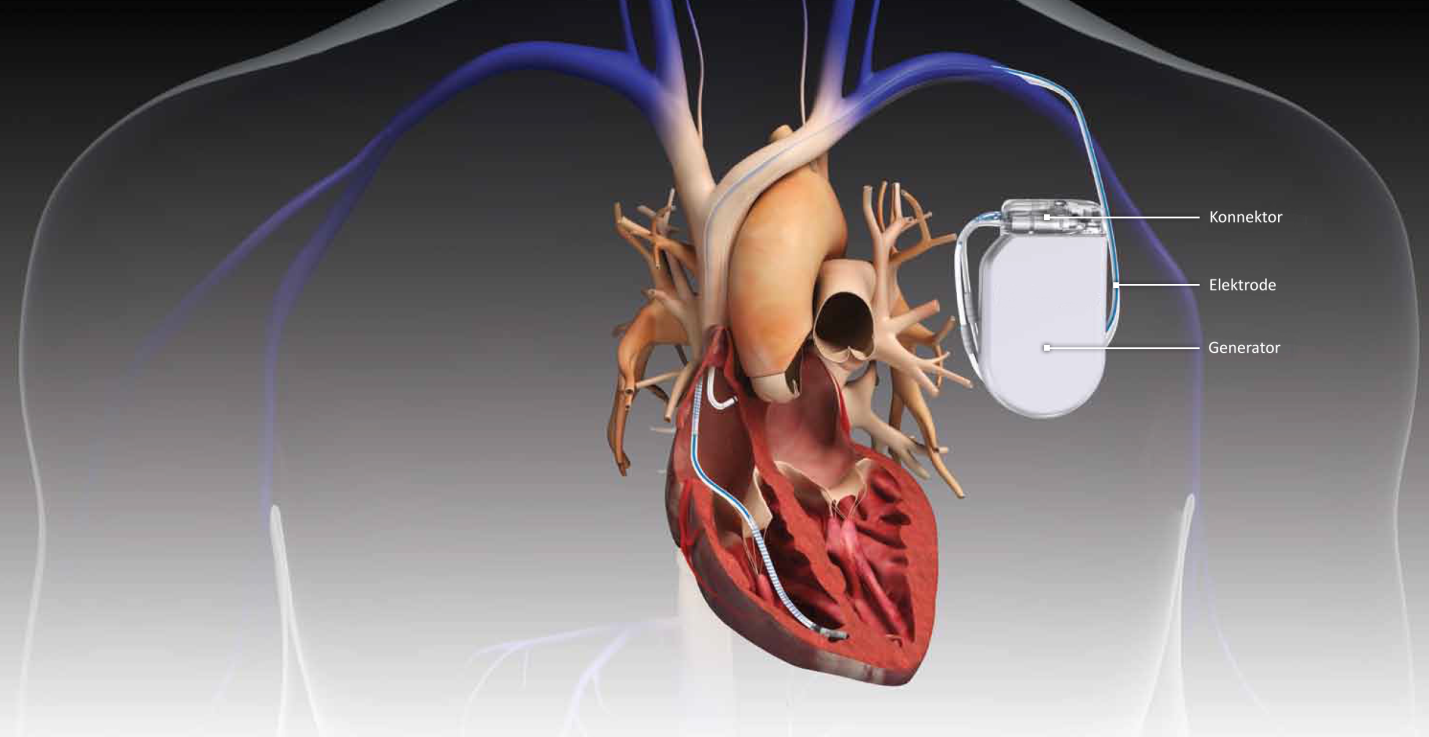
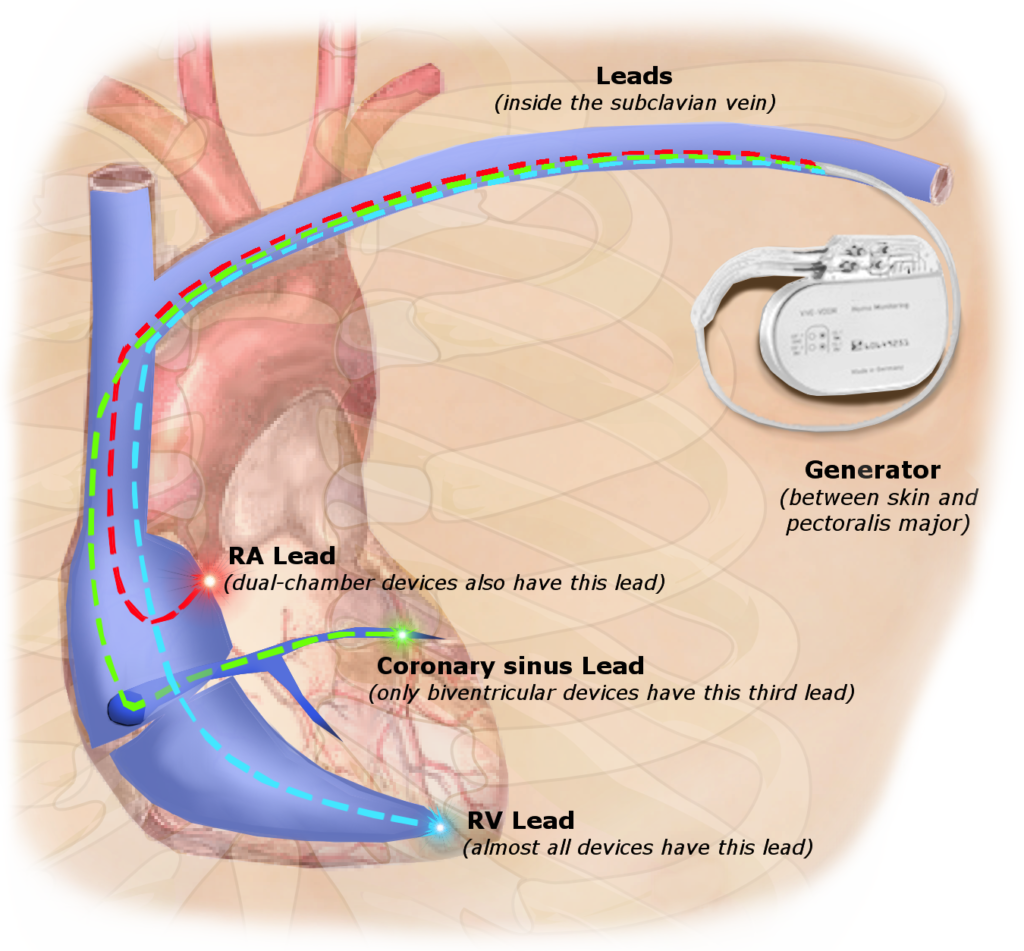
Traditional pacemakers are implanted under the skin, usually near the collarbone, and connected to the heart via leads (wires). They consist of:
• A pulse generator that delivers electrical impulses.
• Leads placed in the heart chambers to transmit signals.
• Electrodes that monitor the heart’s electrical activity.
These devices have been highly effective for decades, but their limitations—such as potential lead fractures or infections—have led to the development of newer, more advanced designs.
Leadless Pacemakers: A Minimally Invasive Alternative
Leadless pacemakers represent a major breakthrough in pacing technology. Unlike traditional models, these devices are self-contained units implanted directly inside the heart, eliminating the need for wires. Studies have shown that leadless pacemakers reduce complications such as lead-related infections, improve patient comfort, and allow for a simpler implantation process. Recent research highlights their success in patients with bradycardia and atrioventricular block. (Reference: Research on leadless pacemakers and their impact on patient outcomes, as discussed in multiple cardiology studies.)
Conduction System Pacing: A More Natural Approach
Traditional pacemakers stimulate the right ventricle, which can cause uncoordinated contractions over time. Conduction System Pacing (CSP) is a newer technique that directly stimulates the heart’s natural conduction pathways—such as the His bundle or the left bundle branch—helping the heart beat in a more synchronized manner. Studies suggest CSP improves heart function and reduces the risk of heart failure compared to traditional pacing. (Reference: Clinical trials exploring conduction system pacing and its effectiveness in improving heart rhythm.)
Wireless, Battery-Free Pacemakers
One of the most exciting innovations in pacemaker technology is wireless, battery-free pacemakers. These devices rely on external energy sources, such as light or ultrasound, to power the pacemaker without the need for a traditional battery. Recent animal studies have demonstrated the feasibility of using optical or ultrasound energy to stimulate heart activity, potentially revolutionizing cardiac pacing in the future. (Reference: Research on wireless pacemakers and their ability to function without a traditional power source.)
The Future of Pacemaker Technology
Pacemakers are evolving rapidly, with several promising advancements on the horizon:
• Longer Battery Life – Future pacemakers may last 15+ years, reducing the need for replacements.
• Self-Adjusting Pacing – AI-powered pacemakers could optimize heart rhythm based on real-time physiological data.
• Biodegradable Pacemakers – Temporary pacemakers that dissolve naturally after use, eliminating the need for surgical removal.
• Remote Monitoring Capabilities – Wireless technology allows doctors to track heart activity in real time, improving early detection of complications.
These developments aim to enhance patient safety, reduce surgical risks, and provide more efficient heart rhythm management. (Reference: Ongoing research in AI-driven pacemaker algorithms and biodegradable cardiac devices.)
Conclusion
The heart relies on precise electrical signals to maintain a steady rhythm. When this system malfunctions, pacemakers offer a life-saving solution. Recent innovations—including leadless designs, conduction system pacing, and wireless energy-based devices—are transforming pacemaker therapy, making it safer, more efficient, and more adaptable to patient needs.
As research continues, the future of cardiac pacing will move toward smarter, longer-lasting, and less invasive devices, improving the quality of life for millions of people worldwide.
Read About : Congenital heart defects and diseases
Visit Us At : https://g.co/kgs/rTqAjgt