I still remember the day my friend Rajesh described his persistent chest pressure as “like a heavy weight on my chest.” After months of enduring this discomfort without any clear answers, he finally got the call from his doctor suggesting he might need angioplasty. That conversation changed his life—and it got me thinking about how many of us might be ignoring our heart’s subtle warning signs. If you’re wondering whether angioplasty could be the solution for you, read on. I’ve gathered insights from personal experiences, trusted medical sources, and real-life stories to help you understand the warning signs and tests that can indicate if this procedure might be right for you.
What Exactly Is Angioplasty?
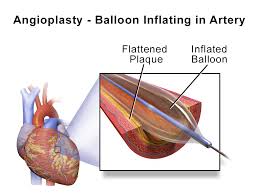
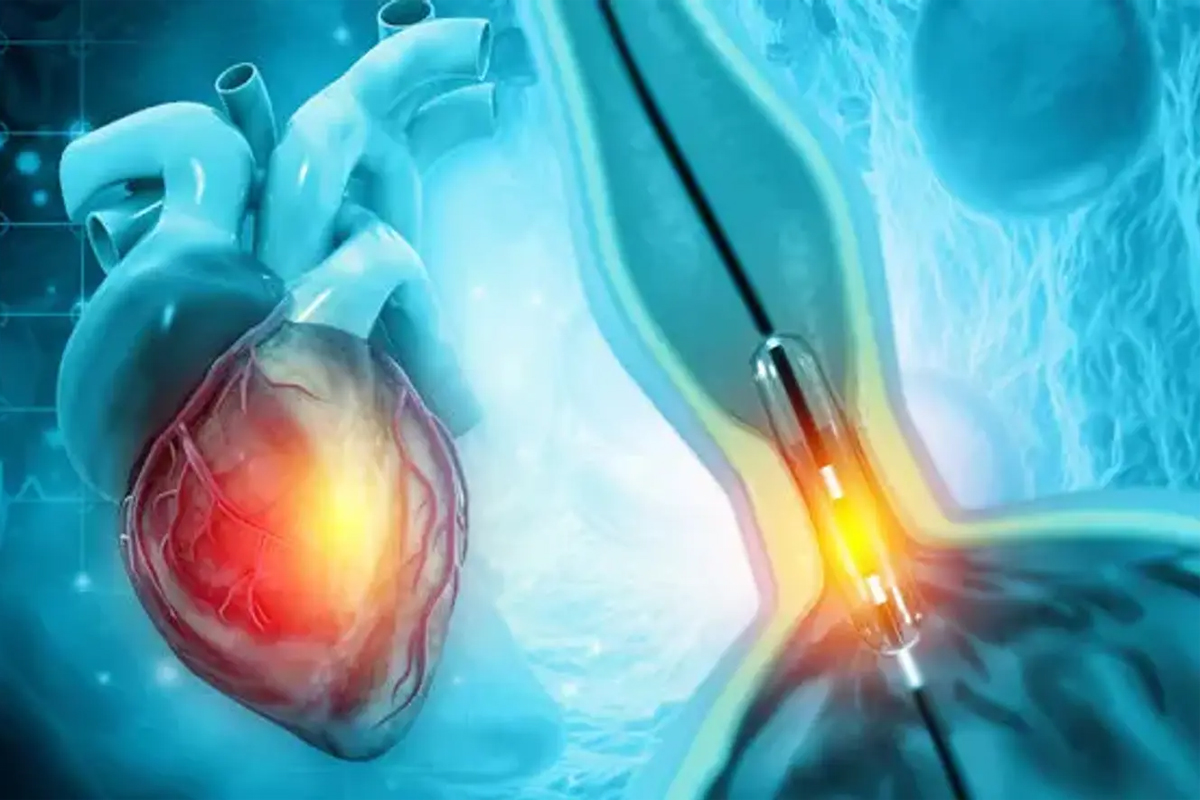
One minimally invasive technique for widening constricted or obstructed coronary arteries is angioplasty. During the procedure, a small balloon is threaded through a catheter into the affected artery. Once in place, the balloon is inflated to widen the artery, and often a stent (a tiny mesh tube) is placed to keep it open. This restoration of blood flow can ease chest pain and reduce the risk of a heart attack.
I recall reading about a patient who, after years of struggling with severe chest pain, found relief post-angioplasty. His quality of life improved dramatically—he could play with his kids again and even returned to his favorite hobby of cycling. It’s clear that this procedure isn’t just about treating a condition; it’s about giving people a second chance at life.
Recognizing the Warning Signs
So, how do you know if you might need angioplasty? There are several symptoms and red flags that doctors look for. Here is a list of the most typical ones:
1. Persistent Chest Discomfort:
If you experience a heavy, squeezing, or pressure-like sensation in your chest that doesn’t go away—even if it seems to come and go—this could be an indication that your coronary arteries are narrowing. I remember a colleague mentioning how he’d often feel a dull ache after climbing stairs, which he initially brushed off until it became impossible to ignore.
2. Shortness of Breath:
Ever found yourself unusually out of breath while doing normal activities, like walking to the store or even talking on the phone? This could be a sign that your heart isn’t getting enough oxygen due to restricted blood flow. It might not seem dramatic at first, but if you notice a gradual increase in breathlessness, it’s time to get checked.
3. Fatigue That Just Won’t Quit:
Unexplained and persistent tiredness can be another warning sign. When your heart struggles to pump blood effectively, your body may respond with constant fatigue. If you’re finding everyday tasks increasingly exhausting, this could be your body’s way of signaling a deeper issue.
4. Other Subtle Symptoms:
Not everyone experiences the “classic” symptoms. Some people, particularly women, may feel nausea, lightheadedness, or pain in their neck, jaw, or back rather than in the chest. These symptoms can be misleading, which is why it’s so important to discuss any unusual or persistent discomfort with your doctor.
The Diagnostic Journey
If you’re experiencing these symptoms, your doctor will likely recommend a series of diagnostic tests to get a clearer picture of your heart’s health. Here’s what you can typically expect:
Electrocardiogram (ECG):
An ECG is usually the first test your doctor will order. This quick and non-invasive test records the electrical activity of your heart and can reveal irregularities or signs of a previous heart attack. I remember being pleasantly surprised by how simple and painless it was to get an ECG done—it’s a small step that can reveal a lot about your heart.
Stress Test:
During a stress test, your heart is monitored while you engage in physical activity, often on a treadmill or stationary bike. This test helps determine how well your heart handles exertion and can identify areas where blood flow is restricted. It’s an eye-opener for many who thought their symptoms were just part of aging or a sedentary lifestyle.
Echocardiogram:
This ultrasound test uses sound waves to produce images of your heart, allowing doctors to assess its structure and function. An echocardiogram can help pinpoint which arteries are narrowed and by how much. It’s a bit like getting a real-time video of your heart in action, offering invaluable details to guide treatment.
Coronary Angiography:
Often considered the gold standard for diagnosing coronary artery disease, coronary angiography involves injecting a contrast dye into your coronary arteries so that X-ray images can reveal any blockages. Although more invasive than the other tests, it provides a detailed map of your heart’s blood vessels, making it easier for doctors to decide if angioplasty is necessary.
Your Doctor’s Role in the Decision
Ultimately, the decision to undergo angioplasty is not taken lightly. It’s a process that involves careful consideration of your symptoms, test results, and overall risk factors. Dr. Anita Deshmukh, a cardiologist I spoke with recently, stressed that “if medications and lifestyle changes haven’t relieved your symptoms, and your tests show significant blockages, angioplasty can be a very effective way to restore blood flow.” Listening to a trusted medical professional is key in making such a critical decision.
Beyond Angioplasty: Embracing a Heart-Healthy Lifestyle
Even if you undergo angioplasty, it’s important to remember that the procedure is just one part of managing coronary artery disease. Long-term heart health requires ongoing lifestyle changes. Here are some steps that can make a significant difference:
• Adopt a Heart-Healthy Diet:
Adopt a diet high in whole grains, lean meats, fruits, and vegetables. Reducing processed foods, saturated fats, and sugars can help maintain healthy cholesterol levels and keep your arteries clear.
• Exercise Regularly:
Every week, try to get in at least 150 minutes of moderate activity. Whether it’s brisk walking, cycling, or swimming, regular activity strengthens the heart and improves circulation.
• Quit Smoking:
If you smoke, consider seeking help to quit. Smoking is one of the most significant risk factors for coronary artery disease.
• Manage Stress:
Practices like meditation, yoga, and deep breathing can help lower stress levels, which is important because chronic stress can harm your heart.
• Follow Up with Your Doctor:
Keep regular appointments to monitor your heart health. This is crucial for catching any potential issues early and adjusting your treatment plan as needed.
References
1. American Heart Association – “Understanding Angioplasty and Coronary Artery Disease”
2. Mayo Clinic – “Angioplasty: When is it Needed?”
3. WebMD – “Symptoms of Coronary Artery Disease and Angioplasty Options”
Our Thoughts
Taking care of your heart is something we all need to make a priority. If you find yourself dealing with chest pain that doesn’t go away, feeling unusually tired, or experiencing shortness of breath, it’s important to have a chat with your doctor about whether angioplasty might be right for you. I know the idea of a heart procedure can be intimidating, but catching issues early can really make a difference in your long-term health. It’s also worth remembering that angioplasty isn’t a one-stop solution. It’s just one piece of the puzzle when it comes to keeping your heart in top shape. Making everyday choices—like eating well, staying active, and managing stress—plays an equally important role in protecting your heart for years to come.
At the end of the day, your heart deserves all the care you can give it. Listen to what your body is telling you, and don’t be afraid to seek professional advice when something doesn’t feel right. By taking small, proactive steps today, you’re setting the stage for a healthier, more energetic tomorrow.
Also Read About : Maharashtra on High Alert as GBS Outbreak Sparks Crisis Warning!
Visit Us At : https://g.co/kgs/rTqAjgt